 Expert registered nurses and midwives are healthcare professionals who can use their experience and expertise in areas such as vital sign observations to provide objective opinions on professional standards of care in medico-legal cases.
Expert registered nurses and midwives are healthcare professionals who can use their experience and expertise in areas such as vital sign observations to provide objective opinions on professional standards of care in medico-legal cases.
One of the most important tasks that nurses and midwives are required to perform for their patients are vital sign observations. Vital signs are measurements of the body’s main functions and include respiratory rate, oxygen saturations, blood pressure, pulse, level of consciousness, pain score and temperature. Once these are recorded on the observation chart, what then? What are the nursing/midwifery responsibilities once observations are charted?
All nurses are bound by the Nursing and Midwifery Board of Australia’s code of conduct for nurses. Adequacy of obtaining vital sign observations and the subsequent escalation of care in response to those vital signs incorporates the code’s principle 2.1 – practise in accordance with the standards of the profession and broader health system [1]. This then leads on to the Australian Commission on Safety and Quality in Healthcare National Standards. National Standard 8 – Recognising and Responding to Acute Deterioration, is the key standard when it comes to vital sign observation and escalation. This standard outlines the minimum acceptable standard for measurement and documentation of vital signs and other observations, escalation of care and communication processes. Nurses and healthcare facilities must legally abide by these standards, otherwise care can be deemed as negligent [1] [2].
Frequent observations key to detecting early signs of deterioration
Frequency of obtaining vital sign observations is one of the most important aspects. While most patients will have their vital signs taken every six hours, Registered Nurses (RN), Registered Midwives (RM) and doctors need to recognise those patients who require more frequent monitoring. This may include those who have had surgery and require post anaesthetic observations, certain medications or infusions and serious illness or injury. Once this has been determined, the required frequency of observations needs to be documented in the clinical record and on the nursing care plan. Failure to complete these more frequent observations can result in the missed detection of clinical deterioration, leading to increased patient morbidity and/or mortality.
The majority of Australian public and private hospitals use Observation and Response Charts (ORCs) that use a ‘track and trigger’ system to aid in timely recognition of clinical deterioration and outline the required steps following identification of deterioration [2] [3]. Nurses and midwives are required to document vital sign observations on their facility’s ORC at the time the vital signs were obtained. Vital sign observations should not be documented on ORC’s retrospectively as this can result in delayed detection of deterioration [4].
Escalation of care needed to prevent adverse events
Assistants in Nursing (AIN) and Enrolled Nurses (EN) are nurses who have completed a Certificate III in Health Services Assistance or Diploma of Nursing respectively [5]. AINs and ENs require indirect supervision by RNs and RMs. If any vital sign observations fall outside the usual parameters for the patient, AINs and ENs are required to immediately notify the RN/RM providing the supervision [6]. The RN/RM then needs to assess the patient and determine what steps need to be immediately taken. Escalation of care varies depending on how abnormal the vital sign observations are.
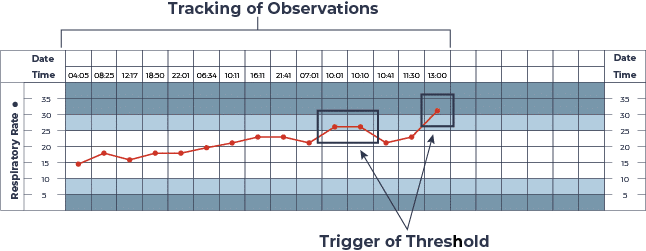
Figure 1: ORC Track and Trigger (CEC, 2022) [7]
The image above is an example taken from the NSW Clinical Excellence Commission [7], showing the trend of a patient’s respiratory rate. The white area shows the normal range for respiratory rate. The yellow and red areas are abnormal. In NSW Health, the yellow area requires the patient be reviewed by the RN/RM and escalation through the clinical review process by a doctor. The doctor is required to review the patient within 30 minutes of notification. If the 30-minute timeframe is breached, the RN/RM will call for a Rapid Response team to review the patient. If an observation falls within the red area, a rapid response team is immediately called. While the RN/RM is waiting for the doctor or rapid response team to arrive, they should commence an A-G assessment and initiate any treatment within their scope of practice. An A-G assessment is a systematic and structured assessment of patient body systems, assessing airway, breathing, circulation, disability, exposure, fluids and glucose [8]. Treatments may include repositioning of the patient, administration of oxygen or administration of medication [7].
Some facilities may have an additional level, Code Blue, to escalate care requirements. A Code Blue can generally be called by someone pressing the emergency button or calling to the hospital switchboard. A Code Blue is called for any patient with a threatened airway or in cardiac arrest. If the patient does not have any limits on their goals of care, staff will commence basic life support until advanced life support trained clinicians are in attendance.
Following these escalation pathways, doctors are required to document the ongoing plan for the patient, including when a follow up review will take place. The RN/RM caring for the patient and the Nurse/Midwife in Charge should discuss and confirm the plan with the doctor/s to ensure that all required investigations and treatments are ordered and completed. If the RN/RM still has concern or the patient remains within or goes back into the coloured area of the chart, escalation will occur again, and the patient will be reviewed by the doctor or Rapid Response team [4].
Failure to escalate: a case study
Let’s look at a case study now and see how failure to complete and/or escalate deterioration in vital sign observations can result in a serious adverse outcome for a patient. Hudson (not real name) was a fit and healthy 21-year-old male who presented to a rural hospital Emergency Department at 1am feeling unwell and coughing up blood. Initial observations showed abnormal vital signs. He had a high temperature, respiratory rate, and heart rate. His oxygen saturations were low, and he required oxygen. He was given an incorrect triage category. His vital signs were not documented on an ORC. If they had been documented, RN 1 would have been alerted to immediately notify a doctor for an urgent review.
Another set of observations were obtained by the RN at 01:05am which again showed Hudson had abnormal vital signs. He also required a higher flow of oxygen than on presentation because of reducing oxygen levels. The RN did not document these observations on an ORC. The RN did notify the doctor of Hudson’s presentation but did not communicate that his vital sign observations required an immediate bedside review by the doctor. The doctor ordered oral antibiotics and to give analgesia. The doctor advised the RN to call him back if Hudson deteriorated. Hudson was admitted to the Acute Ward at 1:15am and an ORC was commenced.
Subsequent observations at 3am and 6am indicated on the ORC that the team leader and doctor needed to review the patient within 30 minutes. The RN did not follow the policy and escalation did not occur. In addition, although the 6am observations indicated that the patient required urgent review, the RN documented that Hudson’s observations were stable.
At 8:43am, Hudson was coughing up blood and the ORC indicated that his observations were abnormal and required urgent escalation to the doctor. The RN escalated to the doctor who commenced immediate treatment for sepsis which included a chest x-ray. On return from the x-ray, the RN called for the Medical Emergency Team due to deterioration of his vital sign observations. Hudson was moved to the close observation bed however continued to deteriorate and at 10:50am was moved to the resuscitation bay. Shortly after, Hudson had a cardiac arrest. Advanced life support was initiated. Unfortunately, Hudson was pronounced deceased at 12:11pm. His cause of death was severe sepsis resulting in pulmonary haemorrhage.
This case study demonstrates that the delay in recognition and appropriate escalation to the doctor contributed to the death of Hudson. The RN who initially cared for the patient appeared negligent in the fact that she did not use the ORC, as set out in hospital, and state policy, and did not escalate care as outlined in the hospital and state policy. Had the RN followed policy, it is likely that appropriate sepsis management would have commenced soon after Hudson presented to the Emergency Department, which potentially would have included being transferred to a tertiary facility for ongoing management.
Expert nurses an advantage in medico-legal cases
Vital sign observations are integral to nursing practice. Without vital sign observations and appropriate escalation when a patient’s condition deteriorates, there can be devastating outcomes. Escalation systems built into ORC’s save patient lives and assist in the decision making and escalation required for nurses [2].
In cases of medical negligence, skills such as these are the reason why there are significant legal advantages in engaging expert nurses and midwives, whose specialised training is ideally suited to conducting forensic medical reviews, determining the causes of illness, producing quality medico-legal reports, and ultimately helping you to prove liability.
Registered Nurse and Medico-Legal Expert
References
1] https://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/Professional-standards.aspx
[4] Brooks, N. (2021). How to undertake effective record-keeping and documentation. Nursing Standard, doi:10.778/ns.2021.e11700.
[5] https://www.skills.vic.gov.au
[8] Recognition and management of patients who are deteriorating (nsw.gov.au)
